- Performing dilation at-home using self-dilation device
- Considering treatment that resolve the narrowing (i.e., stent, laser treatment)
- Temporarily altering the diet to soft or liquid one
- Using a gastric tube for feeding
Laryngectomee Newsletter provides information for laryngectomee and neck breathers how to cope with the corona (COVID-19) pandemic. It advises how to prevent the infection and deal with depression, social isolation, fibrosis, lymphedema, mucous problems, and voice prosthesis leak. It provides suggestions how to deal with esophageal dilation, hospitalization, and keep fit and eat well. Created by Itzhak Brook MD, Professor of Pediatrics at Georgetown University, a physician and a laryngectomee
The Newsletter presents suggestions how laryngectomees can cope with the COVID-19 pandemic.
The Laryngectomee Newsletter is presented by Itzhak Brook MD. Dr Brook is a physician and a laryngectomee. He is the author of "The Laryngectomee Guide for COVID-19 Pandemic", " The Laryngectomee Guide", " The Laryngectomee Guide Expanded Edition", and " My Voice, a Physician’s Personal Experience with Throat Cancer ".
Dr. Brook is also the creator of the blog " My Voice ". The blog contains information about head and neck cancer, and manuscripts and videos about Dr. Brook's experience as a patient with throat cancer.
Wednesday, April 29, 2020
Neopharyngeal or esophageal narrowing during COVID-19 pandemic
Friday, April 24, 2020
Going outside during the COVID-19 pandemic
- Cleaning the stoma and trachea including inserting saline into the trachea and coughing out the secretions before going out
- Taking care of the stoma and it’s secretions at a private location away from others (e.g., bathroom, separate room)
- Covering the stoma (with napkin, cloth or elbow) whenever coughing or sneezing. Preferably this is done away from other people. When coughing forcefully the stoma can produce large amount of droplets that can spread and infect others when the laryngectomee carries a respiratory virus such as COVID-19
- Keeping a distance of at least 6 feet (2 meters) from others
- A useful routine is to use the non-dominant hand to touch the stoma and the dominant hand for other activities (e.g., touching a door handle).
- Wearing a surgical mask or garment over the mouth and nose (in addition another one over the stoma). This is done to protect the laryngectomee from becoming infected, as well as others the laryngectomee is infected. Wearing a mask over the mouth and nose in public prevent the laryngectomee from standing out from others. Wearing the mask on the stoma and face also serves in preventing laryngectomees from touching these locations with unclean hands.
As home confinement and other restrictions are being slowly lifted, it would be prudent for laryngectomees to continue to observe these precautionary measures. As more clinical experience in managing COVID-19 infection is gained and new medications and vaccines are available the consequences of becoming infected may become less dangerous.
Preventing COVID-19 infection in laryngectomees
There have been several laryngectomees who acquired COVID-19 infection. Those who were diagnosed had a broad spectrum of symptoms from minimal to severe. There were at least 2 who also had comorbidities that died from COVID-19 infection.
over the stoma (in addition to the HME). Tie the upper strings of the mask around neck, use additional extension string to connect the two lower mask strings together under the arms and behind the back.
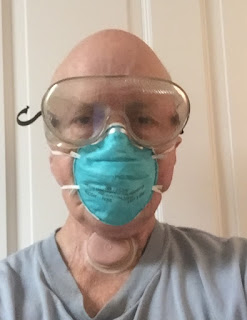
• Wearing an additional surgical mask or respirator over the nose and mouth, and protective glasses or face shield (see pictures below). This can prevent the virus from entering the body through these sites or spread to other people when infected. Men should shave their facial hair prior to wearing surgical mask or respirator. If worn properly, a surgical mask can help block large-particle droplets, splashes, sprays or splatter that may contain germs (viruses and bacteria). While a surgical mask may be effective in blocking splashes and large-particle droplets, it does not filter or block very small particles in the air that may be transmitted by coughs, and sneezes. Wearing the mask on the stoma and face also serves in preventing laryngectomees from touching these locations with unclean hands.
Wearing protective glasses and surgical mask
Additional sources about protection of laryngectomees:
Oral Oncology editorial about protection of laryngectomees
Tracheotomy Education Website: Laryngectomy and Coronavirus Disease (COVID-19)
Message from the Japanese Head and Neck Support Society. (in Japanese and English)
Message from the Singapore Cancer Society
Message from Nu Voice ( University of Southern California) Los Angeles.
Wearing a modified face mask over the stoma
Adequate hospital care of laryngectomees
2. Inform the ward’s head nurse, attending physician and anesthetist (when undergoing a procedure with sedation or surgery) about the proper way of administrating anesthesia, suctioning, ventilating and intubation. Show them the video in YouTube: https://goo.gl/Unstch Show them the video in YouTube: https://goo.gl/Unstch (See video below). The video is available in DVD from Atos Medical.
The National Patient Safety Project has developed an algorithm for emergency management of patients with laryngectomy.
- The kit should contain the following:
- An updated and current summary of the medical and surgical history, allergies and diagnoses
- An updated list of the medications taken and the results of all procedures, radiological examinations, scans and laboratory tests. These may be placed on a disc or USB flash drive
- Contact information and proof of medical insurance
- Information (phone, email, address) of the laryngectomee’s physician(s), speech and language pathologist, family members and friend(s)
- A figure or drawing of a side view of the neck that explains the anatomy of the laryngectomee's upper airways and if relevant where the voice prosthesis is located
- A paper pad and pen
- An electrolarynx with extra batteries (even for those using a voice prosthesis)
- A box of paper tissues
- A supply of saline bullets, HME filters, HME housing, and supplies needed to apply and remove them (e.g., alcohol, Remove, Skin Tag, glue) and to clean the voice prosthesis (brush, flushing bulb)
- Tweezers, mirror, flash light (with extra batteries)
Tuesday, April 21, 2020
COVID-19 testing in laryngectomees
- A viral test tells if someone has a
current infection. It is obtained by collecting a nasopharyngeal specimen (e.g., nasal, oropharyngeal) with a swab.
Neck breathers should be tested in two
locations: by collecting a nasopharyngeal specimen as well as a stomal specimen. Click to see the American Academy of Otolaryngology recommendations.
- An antibody test is obtained by getting a blood sample. It tells if a person had a previous infection.
Sunday, April 19, 2020
Facemasks, N95 respirator and face covers for neck breathers
Monday, April 13, 2020
Beard or facial hair interfere with face mask's efficacy against COVID-19
Thursday, April 9, 2020
Guidelines for head and neck cancer care during COVID-19 pandemic
A special article just published by DrGivi and colleagues in JAMA Otolaryngology-Head & Neck Surgery, presented guidelines for head and neck physical examination and surgical and non-surgical procedures during the coronavirus (COVID-19) pandemic.
- Non urgent appointments should be postponed to limit infection of patients or health care workers. This may include postponing appointments for patients with benign disease and for those undergoing routine surveillance after treatment for head and neck cancer.
- Patients should be queried by telephone about new or concerning signs or symptoms that may indicate recurrence and/or pending issues, as well as symptoms suggestive of COVID-19.
- In-person clinic visits should be offered to those at risk for significant negative outcomes without evaluation.
- Maintaining relationships with patients and support assessments that can be made without in-person examinations. The use of telephone, video, or telemedicine visits should be considered.
- In-person examinations should be limited
to patients who need a thorough head and neck examination ( e.g. postoperative visits,
tracheoesophageal prosthesis complications, symptoms concerning for cancer
recurrence, etc.).Detailed guidelines are provided for physical examinations and associated procedures.
Hennessy et al. present their special considerations and best practice recommendations in the management of total laryngectomy patients. They also presented their recommendations for laryngectomy patients and how to minimizing community exposures.
Friday, April 3, 2020
Coping with COVID-19 pandemic as head and neck cancer patient
- Washing hands with soap and water frequently, for 20 seconds, including wrists.
- If unable to wash hands, using hand sanitizer and rubbing them for 20 seconds.
- Disinfecting commonly used surfaces such as tabletops, doorknobs, and phones.
- Avoiding direct contact with others such as hugging or shaking hands, and staying at least 6 feet away from other people.
- Avoiding being in large groups of 6 or more people, especially when in an enclosed space.
- Avoiding sharing cups or utensils with others.
- Covering the mouth or stoma during a cough or sneeze.
- Wearing a face mask and protective glasses when at risk of exposure to the virus
- Avoiding contact with anyone with a known COVID-19 infection or individuals with a cough and/or fever.
- Avoiding air travel or other public transportation.
- Notifying their doctor immediately when feeling sick (develop a cough, fever, muscle aches, or other symptoms) or if after having contact with anyone with a known or suspected COVID-19 infection. It may be necessary to be evaluated and potentially tested for the virus.
While social distancing, isolation, and quarantine at home are effective in reducing the incidence of COVID-19, they do increase health risks from other causes. Social isolation among older adults is associated with heightened risk of cardiovascular, autoimmune, neurocognitive, and mental health problems. It is therefore important that individuals do not neglect their medical problems during the pandemic.
- Maintaining close communication with family/loved ones and health care team
- Having a sufficient supply (at least a 2-week supply) of easy to preserve food items, prescriptions and cleaning supplies and other essentials.
- Contacting one’s physician to ensure one has adequate access to prescription medications, and necessary supplies (e.g., tube feedings, tracheostomy supplies and personal protective equipment)